Wherever treatment outcomes are measured, quality improves dramatically. Unfortunately, systematic measurement of patient outcomes remains the exception.

Facts count: Unique knowledge of treatment success
Facts offer security; figures provide perspective. This is particularly true in the phase between diagnosis and therapy, when patients face uncertainty about the decisions facing them. With this in mind, we would like to outline the documented outcomes of our treatments.
Michael E. Porter
Economist at Harvard University, Cambridge, MA, USA
One of these exceptions is the Martini Clinic
The Martini-Klinik is one such exception. We document our treatment outcomes with the utmost precision, analysing them both for research purposes and to enable all our surgeons to reflect on the outcomes they achieve in terms of continence and potency. In most hospitals, surgeons never learn the outcomes of their treatments because patients return to their usual doctors for post-operative care.

Accompanies you through this topic
PD Dr. Felix Preisser
Consultant
Your questions are welcome
info@martini-klinik.de
+49 (0)40 7410-51300

Improving the treatment
Highly specialized, empathetic and scoring high in outcome quality: Our Prostate Cancer Center.
05.24 minutes
We receive information from former patients who respond to our annual surveys about their quality of life. At present, we correspond with more than 34,000 former patients each year.
We continuously update data on patient outcomes, including cure rates and quality of life, so that we can give our current patients up-to-date figures on the success rates of different treatment options. However, thanks to our clinic’s close ties with science and research, we also compile a range of other data and interesting statistics, which we have collected for you on this page.
We are constantly evaluating clinical and pathological data. This is an ongoing process, which means that outcome figures are dynamic and may change over time as our analysis continues.
Incomparable... well, not quite
We have been measuring outcomes since 1991. Unfortunately, there is a scarcity of data from other organisations for us to measure and compare our clinic against. In light of this, we were pleased that Barmer, a statutory health insurance provider in Germany, published data on all its prostate cancer patients in 2012. These are the comparable figures:
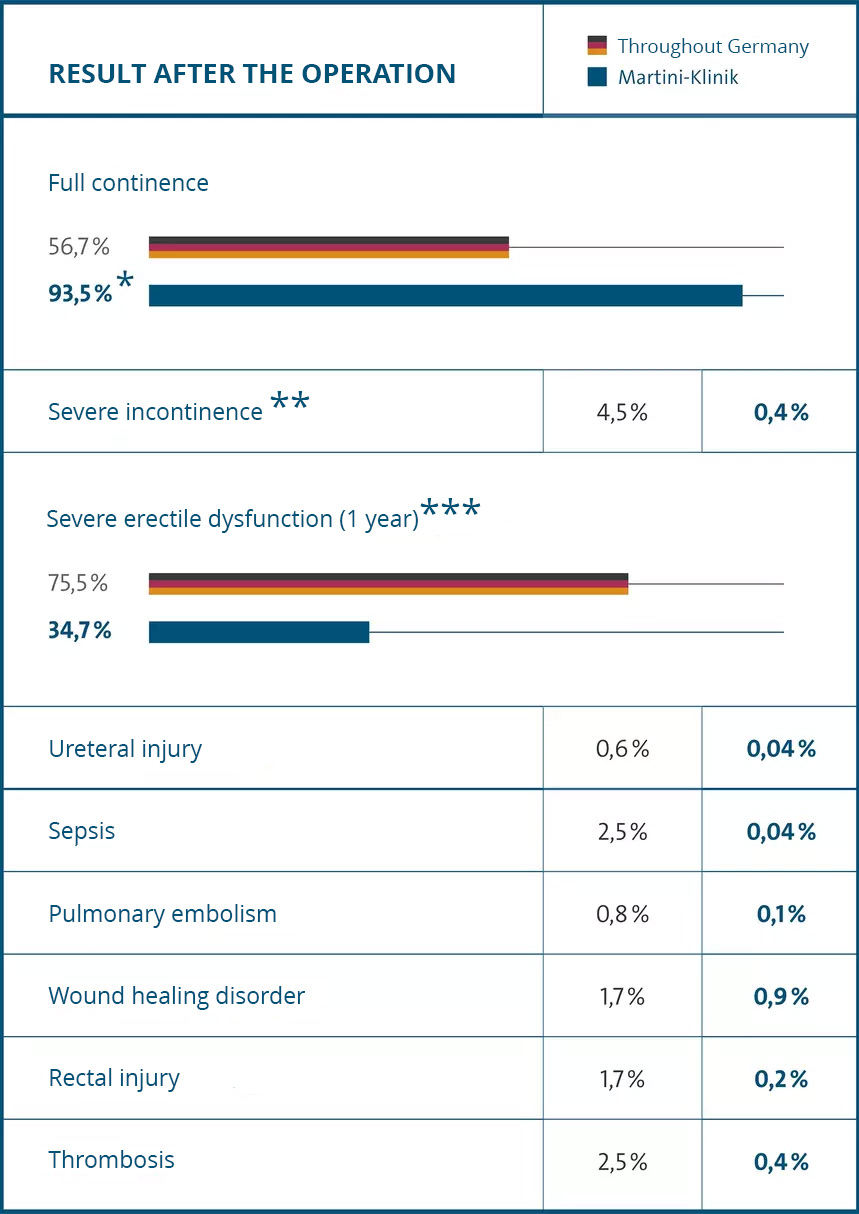
* Full continence is defined as: no pads required, or only used as a precaution
** More than five pads used per day
*** Includes patients with impaired potency prior to surgery
Source: BARMER GEK Hospital Report 2012 [in German], Martini-Klinik database
Published in “Case Study: Martini Klinik: Prostate Cancer Care” by Michael E. Porter, Jens Deerberg-Wittram and Clifford Marks, Harvard Business School
What are the chances of being cured?
As a prostate cancer patient, the word “cure” means completely removing the prostate cancer from your body, either through surgery or by completely killing the cancer through radiotherapy. Treatment should always strive to have the smallest possible impact on a patient’s quality of life.
A patient is usually considered as “cured” when they do not experience a recurrence of prostate cancer (also known as a relapse) for at least five years. This can be monitored effectively following prostate cancer treatment by measuring a patient’s PSA level. Other instrument-based examinations (i.e. MRI/CT scans, scintigraphy) might be used depending on your personal circumstances.
The outcomes outlined here are the results of over two decades of continuous clinical quality control. This is why the doctors at the Martini-Klinik are keen to hear from former patients about how they are doing, what their quality of life has been after treatment and whether their cancer has been cured. In addition to our interest in our patients’ wellbeing, even years after their treatment at the Martini-Klinik, this allows us to draw conclusions about future patients’ chances of being cured and maintaining a good quality of life.
Facts about biochemical recurrence-free patients
Following complete removal of the prostate in by means of radical prostatectomy, a patient’s PSA level usually falls to zero because there is no more tissue left to produce the prostate-specific antigen (PSA). However, if a patient has a PSA level of 0.2 ng/ml or higher after surgery, this indicates recurrent tumour activity. This is known as biochemical recurrence. It is not automatically a life-threatening condition. It may indicate that further treatment is required, such as postoperative radiation or hormone therapy.
Health our patients after 10 years | ||||
| *1 Disease-specific survival *2 Biochemical recurrence-free | *1 | *2 | ||
| pT2 | Tumor not spread | 98* | 87% | |
| pT3a | Tumor infiltrated capsule | 98* | 53% | |
| pT3b | Tumor infiltrated seminal vescicles | 87* | 28% | |
| pT4 | Tumor infiltrated other tissue | 77* | 6% | |
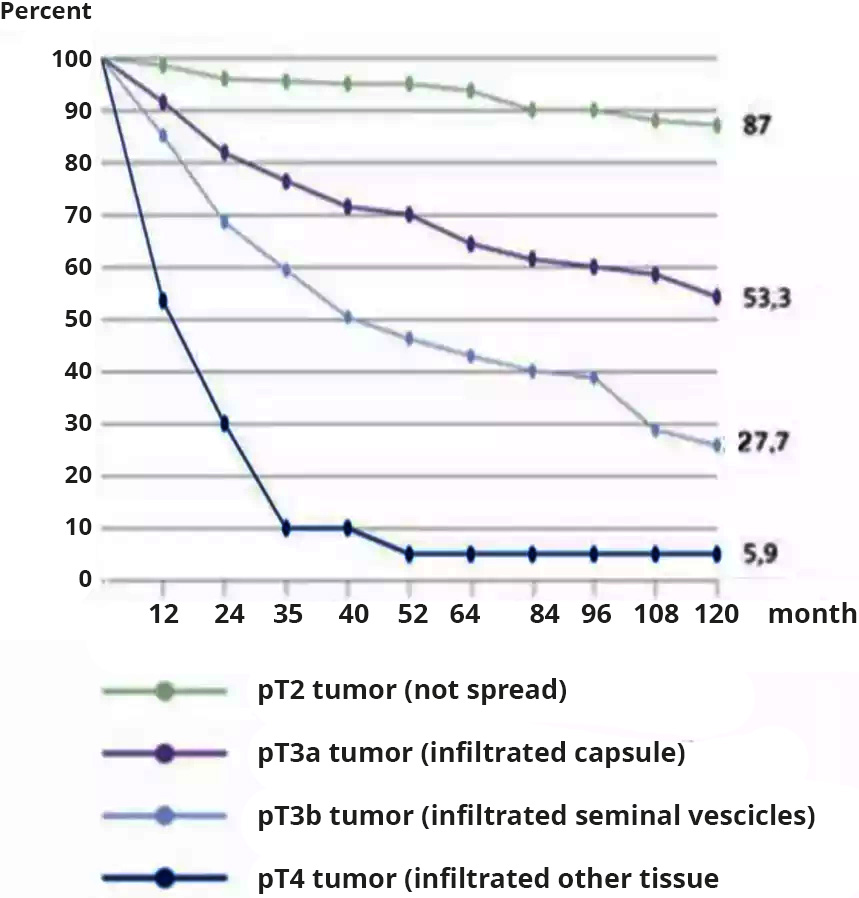
This graph shows numbers of biochemical recurrence-free patients following a prostatectomy. Source: Isbarn, H., et al. (2009)
Biochemical recurrence-free survival following radiotherapy
Relapses are harder to identify than following surgical treatment.
A patient’s PSA level remains the most effective marker for assessing whether their cancer has been cured following radiotherapy or brachytherapy (LDR or HDR). However, the significance of a patient’s PSA level differs following radiation-based treatment. It is not common for the PSA level to actually reach “zero” – as is the case following radical removal of the prostate – because the patient retains their prostate, which means that PSA-producing tissue is still in their body. With this in mind, relapses are harder to identify than following surgical treatment. Nevertheless, the long-term process of curing cancer with brachytherapy is similar to that of complete removal of the prostate. In addition, the cure rate for radiotherapeutic treatment methods also depends on how early the tumour is detected. The earlier it is detected, the higher the cure rate following brachytherapy.
More facts about disease-specific survival
Ultimately, for you as a patient, the crucial question is disease-specific survival: what are the chances of surviving prostate cancer? With this in mind, Dr. Hendrik Isbarn evaluated figures from our clinic again four years later, which confirmed the trend in the figures shown in the graph above. Fundamentally, the latest figures back up this trend.
- If the tumour is confined to the prostate (pT2) or has “only” extended beyond the prostate (pT3a), more than 98% of men survive the disease for at least 10 years.
- If cancer cells have already reached the seminal vesicles (pT3b) or the tissue surrounding the prostate (pT4) the figures are 87% and 77% respectively.
- If the lymph nodes have been affected (pN+), 81% of our patients survive.
- The disease-specific survival rate for patients with a PSA level > 20 ng/ml was 93%.
- The survival rate for patients with a Gleason score of 8 or higher was 70%.
“Wherever treatment outcomes are measured, quality improves dramatically. Unfortunately, systematic measurement of patient outcomes remains the exception,” says Michael E. Porter, economist at Harvard University, Cambridge, MA, USA. The Martini-Klinik is one such exception. We document our treatment outcomes with the utmost precision, analysing them both for research purposes and to enable all our surgeons to reflect on the outcomes they achieve in terms of continence and potency. Unfortunately, there is a scarcity of data from other organisations for us to measure and compare the clinic against. However, we have identified a few comparable figures.